
Become a Veterinarian Assistant and Work with Animals!
Becoming a veterinarian assistant opens a door to animal healthcare that is far more accessible than earning a vet tech or veterinary degree. Vet assistants work closely with pets every day and perform a wide variety of tasks that help vet clinics and hospitals run smoothly.
If you discover you love the work and want to pursue a vet tech degree, working as a vet assistant gives you valuable experience and a chance to save money for school.
With no advanced education or licensing requirements, a vet assistant position allows you to be part of a team that helps pets live long, healthy, happy lives. However, a lot of people compete for veterinarian assistant positions, so landing a job without any experience or education can be tricky.
Most clinics can afford to be choosy when they’re evaluating job applicants. To beef up your resume, it’s a good idea to earn a vet assistant certificate. Doing so will teach you about animal health, animal behavior and safe handling, surgical prep, clinic etiquette, small animal nursing and more. Having such knowledge can make you a much more attractive job candidate.
Finally a Vet Assistant School Near Me!
It can be hard to find a brick and mortar school where you can earn a veterinarian assistant certificate. Google “vet assistant schools near me” and you will likely turn up only online programs. This is not a problem; and when you learn the advantages of earning your veterinary assistant certificate online, it’s easy to forget all about brick and mortar schools.
Of all the vet assistant programs online, Animal Behavior College ranks among the top schools. We offer a stellar hybrid program that combines online learning and real-world experience, providing a solid career foundation.
Becoming a vet assistant checks all the boxes if you love animals and are interested in helping them live healthy lives without taking a vow of poverty. If you dream of working closely with animals, being part of a veterinary team can be fulfilling and rewarding.
Enrolling in our vet assistant program is a giant-sized step toward realizing your dream.
How to Become a Vet Assistant
Our NAVTA-approved veterinary assistant program is designed to teach you all the skills you need to pursue your dream career. Our online program is available to all students anywhere in the United States or Canada with access to an internet-enabled device!
Ours is one of only a few online programs to be approved by the National Association of Veterinary Technicians in America (NAVTA).
ABC is more than just an online school; we’re technically a hybrid, combining online learning and a real world mentorship (called an “externship”) in a veterinary facility. During the externship students get to put what they learned online into practice. We have thousands of veterinary clinic partners, so students can get experience locally.
ABC teaches you the requirements necessary to become a more attractive job candidate and the externship instills confidence in your newfound skills. Having a veterinary assistant certificate can give you an advantage when applying for jobs.New updated program! Updated and revamped, our new Veterinary Assistant Program curriculum is now available to all students and alumni!
Learn more about our program by calling 800-795-3294 or enroll now online!
Vet Assistant Career Earning Potential

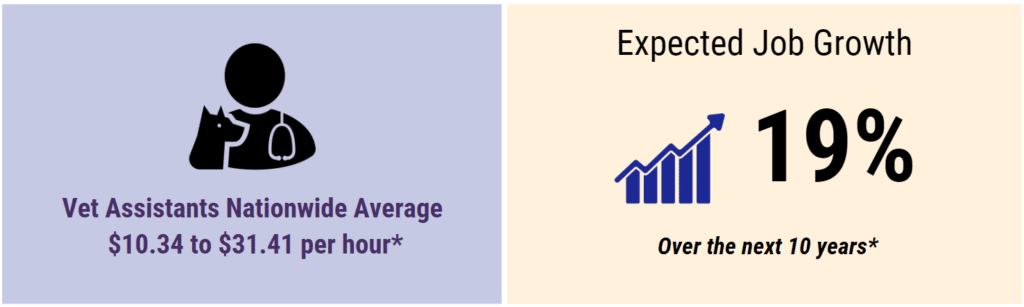
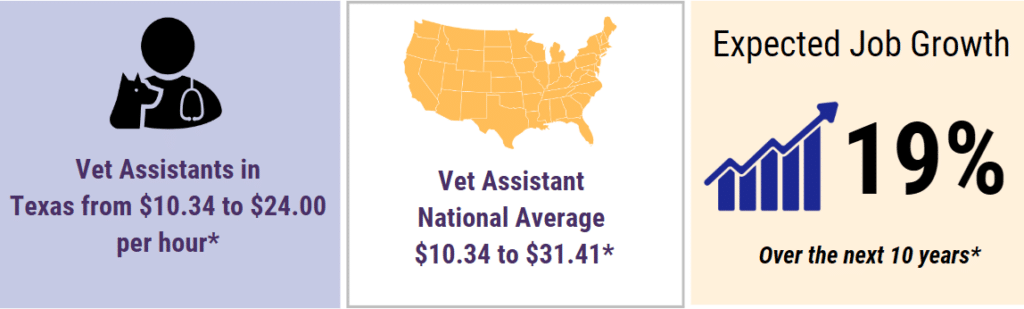

*Source: Bureau of Labor Statistics, Salary.com & Indeed.com 2024. Hourly rates may vary in your area.
Designed to prepare you for a career working with animals, our program teaches you everything from exam room prep and surgical procedure to small animal health care. After successful completion of the prior stages, you’ll then be placed in a veterinary environment to complete your externship.
Our Veterinary Assistant Program makes it possible to:

- Get your post-secondary education online
- Acquire practical skills you can apply in real-life settings
- Receive Pet CPR and First Aid Certification
- Experience what it’s like to work in a veterinary hospital
- Receive ongoing student support
- Invest in your future doing what you love
- Receive digital study materials
- Earn your vet assistant certificate
Switching careers doesn’t necessarily mean you quit your day job to return to school. Our online coursework fits easily into any schedule. Make your childhood dream of helping animals a reality at ABC.
NAVTA-Approved Curriculum

Why enroll in any other program when you can learn at a NAVTA-approved vet assistant school? Our curriculum is annually reviewed by registered veterinary technicians who have had decades of experience working with animals. Given the high regard, the veterinary community has for the NAVTA approval, getting your ABC veterinary assistant certificate may be the right step toward your career.
Real World Training & Mentorship
Experience is an important component of our program. We have relationships with more than 5,600 veterinary facilities across the U.S. and Canada. This allows us to arrange local externships for our students, providing the opportunity to real world experience.
During your externship, you’ll be given the opportunity to interact with professionals in the veterinary industry and have real world experiences with animals. Hundreds of mentors in veterinary offices across the country partner with ABC.
Tuition & Financing
Tuition ranges from 1,199.00 $1,086.60 to $5,630.00 depending on your chosen payment plan. * This cost covers all learning materials, including the real world training externship.
*Ask about our discount for Active Military and Veterans who enroll in our distance learning courses
Military Spouses May Qualify for Free Tuition

Are you a military spouse? You may receive up to $4,000 toward your tuition costs, including course materials and externship. ABC has years of experience working with military spouses and we understand the importance of a portable career. Learn if you qualify for this educational benefit through Military Spouse Career Advancement Accounts (MyCAA) by calling Animal Behavior College directly at 800-795-3294.
Flexible Schedule & Online Study
Learning can be easy when you can access the entire curriculum online. Complete our veterinary assistant course no matter where you live within the United States or Canada. One of the best parts of our online program is you can study on your own time. Flexible scheduling may afford you the opportunity to keep your current job, balance home life and pursue a career as a veterinary assistant.
Always Located Near You
No matter where you live, or where you’re transferred to within the U.S. or Canada, Animal Behavior College is available to you. Given our network of over 5,600 veterinary facilities, we’re able to offer you this real-world training experience.
Student Support From Professionals In The Field
Stay on track with the help, guidance and support of our ABC Program Manager team. Each Program Manager is a Registered Veterinary Technician (RVT) who has years of personal on-the-job working experience in a veterinary facility. This means as you go through the program, you will receive the benefits from their years of animal handling and veterinary experience.
Approved Veterinary Assistant Program

Upon successful completion of the program, you’ll become an Animal Behavior College Veterinary Assistant (ABCVA). Earning your certificate through our NAVTA-approved program demonstrates your knowledge in the veterinary field to potential employers.
New & Improved Veterinary Assistant School Curriculum
Animal Behavior College prepares you for a career in the veterinary field. We have worked tirelessly to recently update our Veterinary Assistant Program curriculum to provide you with the most up-to-date education and industry information. You’ll learn the fundamentals and requirements necessary to work in a veterinary hospital or clinic then you will gain real world experience during your externship.
- Stage 1 Office Etiquette & Hospital Procedures: Explains the various roles of each veterinary team member. Learn how to work in a professional animal hospital environment.
- Stage 2 Animal Behavior and Handling: Focuses on understanding animal behavior and body language, and proper handling and restraint procedures for both canines and felines.
- Stage 3 Examination Room Procedures: Covers basic examination room preparation as well as patient background and physical examination procedures.
- Stage 4 Pharmacy & Pharmacology: Educates about the different aspects of the veterinary assistant’s role in filling prescriptions, administering drugs, accurately dispensing medication and talking to pet owners to make sure they understand their pets’ prescription(s) and how to safely administer them at home.
- Stage 5 Surgical Preparation & Assisting: Describes your responsibilities before, during and after a surgical procedure.
- Stage 6 Small Animal Nursing: Teaches about common procedures the veterinary assistant completes when nursing patients back to health.
- Stage 7 Laboratory Procedures: Learn how to prepare samples for analysis, conduct simple laboratory tests, and record the results accordingly as requested by the veterinarian.
- Stage 8 Radiology Ultrasound Imaging & Endoscopy: Discover the knowledge essential for assisting in veterinary diagnostic imaging.
- Stage 9 Career Building: Guidance on choosing the right career and facility, searching for a job, creating an exceptional cover letter and résumé, excelling during any type of interview, setting yourself up to succeed on the job and maintaining your new career long term.
- Stage 10 Externship: Gives you invaluable on-the-job training experience at a veterinary hospital.
- Stage 11 Final Exam & Graduation
Pave the Way to a Veterinary Assistant Career Today
Animals are always in need of your help and some employers may welcome job applicants that have earned their certificate through a NAVTA-approved program. You can make a difference in the lives of animals. Stop dreaming and start doing.
Please note: Animal Behavior College does not guarantee employment after graduation.
*Additional shipping and handling charges may apply.
Save
Veterinary Assistant Career Resources

Career Information and Advice for Vet Assistants from the professionals at Animal Behavior College





